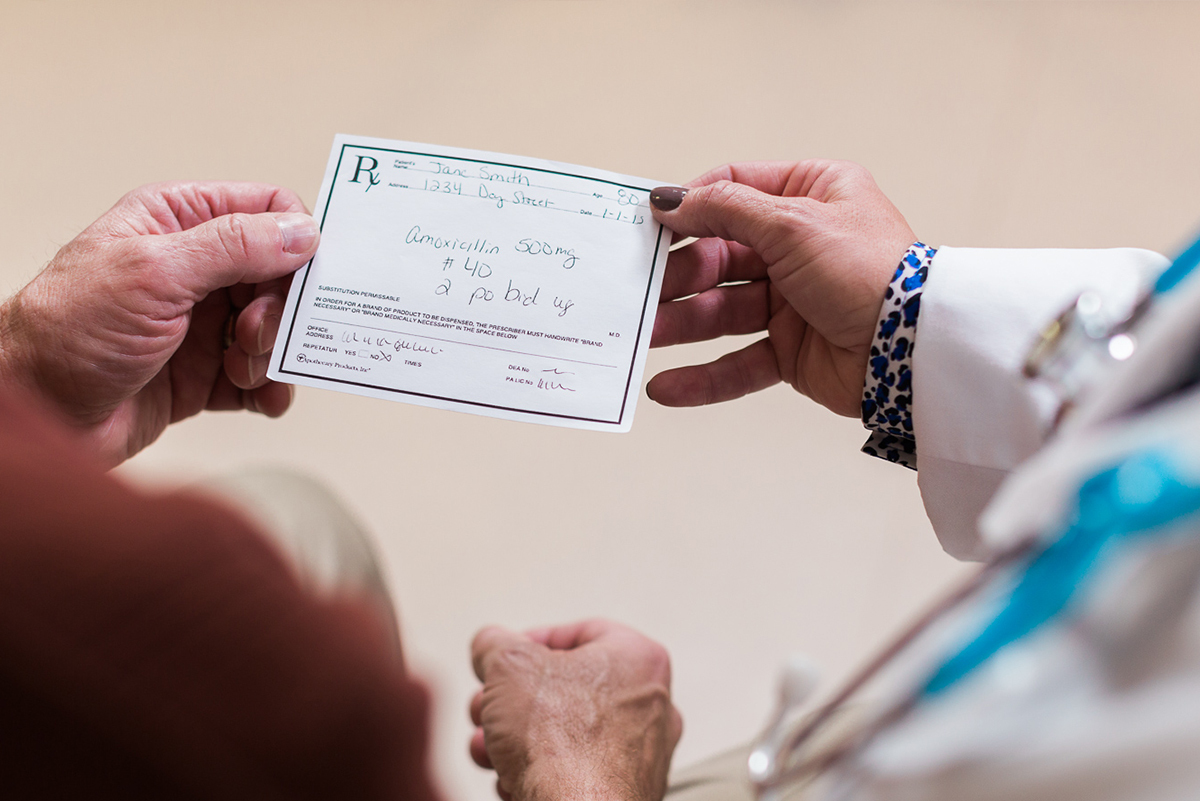
Managing a prescription regimen can feel daunting for older adults, especially if they are managing multiple conditions and see more than one doctor. A pharmacist is a key, but sometimes overlooked, player on an aging adult’s healthcare team. They are an excellent source of information for medication, both prescription and over-the-counter.
In order to manage prescriptions and over-the-counter drugs safely and help alleviate stress and reduce potential hazards, older adults and their caregivers should ask the pharmacist these key questions.
Another consideration to discuss with aging loved ones is the need or desire to have more help at home. Professional caregivers can help with medication management, meal prep and other household duties to make aging in place a safe and viable option.
Keep an up-to-date list of all the medications you or your aging loved one take, their dosages, and the reason for taking them and carry it with you.
A “Caregiver’s Notebook”—a looseleaf binder maintained by a caregiver—is an ideal way to compile information on medical diagnoses, doctors’ appointments, questions, and medication history, according to the Family Caregiver Alliance (FCA). Sharing your updated list every time you see your doctor, nurse, pharmacist, or other healthcare provider helps them give you the best care possible. It could even prevent a dangerous medication situation. Unfortunately, medication mismanagement is one of the more serious health threats facing older adults.
It’s important to find out up-front if the medication is a short-term or long-term regimen that could require lifestyle changes. It’s also important to be aware of expiration dates as certain medicines like insulin or antibiotics are sensitive and could lose efficacy.
All medicines have the potential to cause side effects. Ask the pharmacist what to expect and the most frequently reported effects particularly for older adults. For instance, if a medication causes drowsiness, it can make an older adult more prone to falls or less alert while driving. Certain medications can cloud memory, which could compound memory issues for someone living with Alzheimer’s. Some antidepressants can cause insomnia and diuretics can affect bathroom habits. Know the 10 signs medications could be to blame for an older adult’s changing health issues.
Most medicines have a dosing schedule (i.e. once a day, three times a day, etc.). For the medicine to be most effective, it may be important to take it around the same time each day. Keep in mind that it’s easy for older adults managing multiple medications to become confused. A dosing schedule can help. Mealtimes or bedtimes can be used as cues for scheduling medication if mealtimes and bedtimes are regularly scheduled. Doctors and pharmacists can assist in developing a plan to best suit a personal daily schedule.
Whether it’s advised to make up a missed dose depends on the drug. Ask your pharmacist his or her advice when you have the prescription dispensed. If you realize that you may have taken a dose incorrectly, notify your physician immediately. And don’t hesitate to ask the pharmacist for ideas on how to remember doses.
Pharmacists often can provide a variety of special pill boxes or other aids that remind an older adult or caregiver to take medications. The devices range from low-tech, such as simple containers with compartments labeled for meals and bedtime, to high-tech, such as containers that beep when it’s time for a dose, or a special bottle cap that counts openings of a prescription bottle to tell if the day’s doses have been taken, according to the FCA.
Pharmacies may also be able to offer prescription labels in large print for those with vision impairment or easy-open bottle tops for clients with arthritis or disabilities. Don’t feel guilty asking the pharmacist for alternatives. And, don’t forget alarm features on smart phones or virtual assistant devices (Google Home or Amazon Echo) or in the home.
Never begin taking a new medication without asking your pharmacist if it will interact with your other medicines, supplements, or even foods. Even “natural,” herbal products contain ingredients that can also cause significant interactions with prescription medication. And foods like grapefruit and ones that contain Vitamin K, are known to interact with certain drugs. For instance, grapefruit can slow the metabolism of some medicines, so it increases the drug levels in your body. Vitamin K, which is found in leafy green vegetables, helps the body with blood clotting but can interfere with blood-thinning medications.
Find out if the medicine requires refrigeration or storage away from heat and light. Even under-the-cabinet lighting is a source of heat, which can damage some medicines. Many medicines require a cool, dry area for storage. Always make sure medications are stored safely away from young children.
Older adults may not feel comfortable going into a crowded pharmacy if illnesses in their local community are rising. Some major pharmacies, like Shoppers Drug Mart and Rexall offer medication delivery, which eliminates the need to pick up prescriptions in person. Many also have pharmacists on-call 24/7 and don’t forget to consider a telehealth visit with your doctor if you have questions. When choosing an online pharmacy, be sure to do your research.
Older adults are at higher risk for certain illnesses like COVID-19, influenza and shingles. Always consult your healthcare provider to find out which vaccines are recommended. Many vaccines are available through the pharmacy.
In-Home Care for Chronic Conditions
Living with a chronic health condition can feel overwhelming. Home Instead skilled Care Professionals relieve the burden with person-centered care tailored to individual needs.